Precision Medicine
Developed by researchers at Boston Children’s Hospital, Harvard, Northeastern, Oxford and other academic organizations, the new dataset offers researchers access to more than 5 million anonymized cases from more than 100 countries.
ARIA will be used to quickly identify and fund transformational science and technology.
Artificial Intelligent
The research team noted that lung tissue gets stiffer as a person gets older, showing different patterns of gene expression than in younger people.
Machine Learning
AdventHealth, Advocate Aurora, Northwell, Novant, Providence and Tenet are just some of the major providers collaborating on the new data platform, whose goal is to "improve health equity and advance personalized medicine," according to its CEO.
Vaccines by six developers – Sinopharm, Sinovac, Pfizer-BioNTech, Moderna, Oxford-AstraZeneca, and Sputnik V (Gamaleya Research Institute) – are the ones doing the rounds in the region. Here’s what’s known about them.
The use of realistic health record information that mimics lifelong medical histories can enable more innovative algorithms for disease modeling.
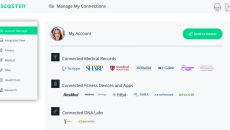
New features include enhanced security with Microsoft Azure Key Vault and Istio Service Mesh and scalable storage for EHR documents, images and DNA sequence files.
SPONSORED
AI-powered clinical decision support enables clinicians in improving quality of care by reducing unwarranted variations.
From vaccines to virtual care, enterprise imaging to precision medicine, these are the growth areas that will shape the direction of healthcare, this year and beyond.
Also, a £10 million research investment made in early stage cancer detection.