news
Home hospitalisation, tech-enabled preventive care, and genomic data-driven personalised care are some of the emerging trends in care in the Asia-Pacific region.
Dr Deok-Hyun Han, Vice CMIO of Samsung Medical Center, Oscar Lee, professor and vice superintendent of China Medical University Hospital, Low Cheng Ooi, associate professor and CTO of Sheares Healthcare, and Dr Mohammad Adib Khumaidi, president of the Indonesian Medical Association, sat together in the closing panel discussion "The Next Wave in Care" at HIMSS23 APAC.
Future of telehealth, harnessing patient data
"[The] COVID-19 pandemic has substantially accelerated the speed of a digital transformation at least by 10 years, meaning that we now have all appreciated the strength of telehealth," shared Prof Lee.
For him, some applications of telehealth will be further developed post-pandemic, such as the growing trend of home hospitalisation as seen in the United States. "Patients don't have to [travel] all the way to be hospitalised and then centralised in the hospital. They can be treated at home – that's the next wave of care that I see."
Prof Lee also noted the "rapid advances" in wearable health technologies, which have allowed people to get a hold of their physiological data.
"But how will we make sense of the information generated by wearable devices?" he asked.
Pondering the same question, Dr Han said it remains a challenge for providers to efficiently collect and analyse a patient's everyday data for preventive care.
"While we generally have detailed data at the earliest from an individual's healthy phase, that [data] remains [inaccessible]," he noted.
In managing volumes of data that health systems can now tap into, empowering patients to become transparent with, as well as knowledgeable about their condition, is imperative.
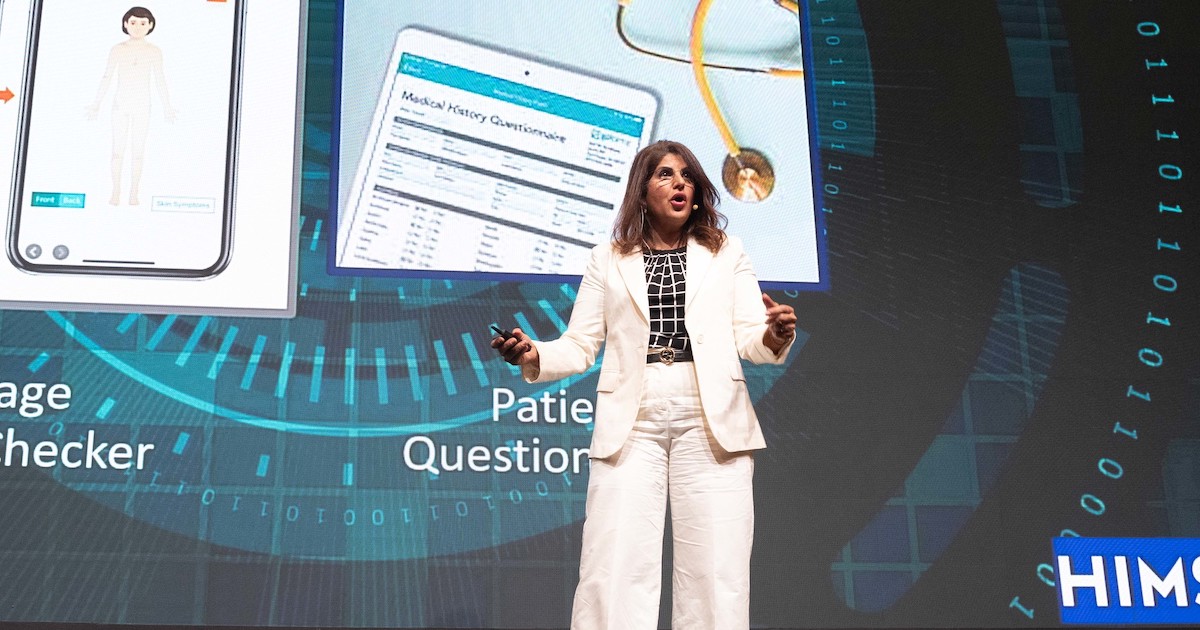
"Patients need to clearly communicate their conditions to their healthcare providers to [allow them to] make enough informed decisions. They must [also] understand the relevant medical details to receive proper care," Dr Han said. To this end, SMC has come up with several initiatives, including their mobile admission process and mobile questionnaire system.
"Patient engagement, though very challenging, is crucial for qualified care."
Technology that cares
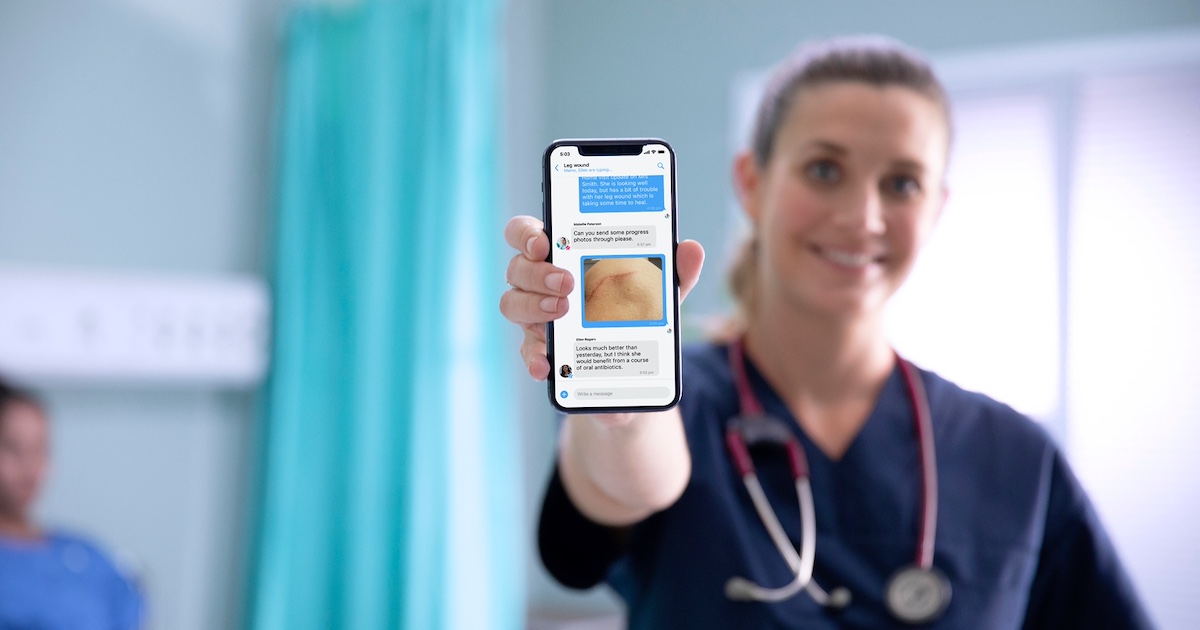
A/Prof Low sees that the next wave in care is "technology [bringing] care to the patient," enhancing particularly the patient experience.
"Patient experience is not just about talking to the doctor. It is the experience of once you find out what illness you have, how you navigate the system, how you find your way to the right specialist, how you get care that is affordable, and how you get the care that is of high quality. [Patient experience is], in a way, where you can have a good relationship with the doctor to explain everything to you…"
Sharing their lessons from the recent pandemic, Dr Khumaidi emphasised that every stakeholder in the health ecosystem – from providers, payers, and policymakers to patients and their families – must have a better understanding of the concept and technology behind personalised medicine.
Additionally, the appropriate patient consent regarding the use of genomic data, which has seen increased collection in recent years, must also be ensured.
"[Genomic data-based] personalised medicine is the new treatment paradigm," he declared.
However, there must be some sort of guideline or ethical considerations in providing such kind of care, Dr Low advised.
"This kind of guidance [falls] to some extent at the national level, at the policy level, and at the ministerial level. But even within the professional bodies themselves, we need to be able to be cognisant of the validated scientific [evidence] before we can make that as a recommendation."
With the influx of new health technologies in the market today, healthcare providers are further reminded to remember their purpose before jumping the gun and implementing them.
"The next wave is not about adopting the technology but what you are trying to achieve with the technology," A/Prof Low said. "We should be employing all the different types of technology to bring [care to the] personal level."
"At the end of the day, [our goal is to] achieve person-enabled health. The role of the hospital will further transform from treating diseases to health promotion so that we make [everyone] in the community not only live longer but also healthier," Prof Lee said.