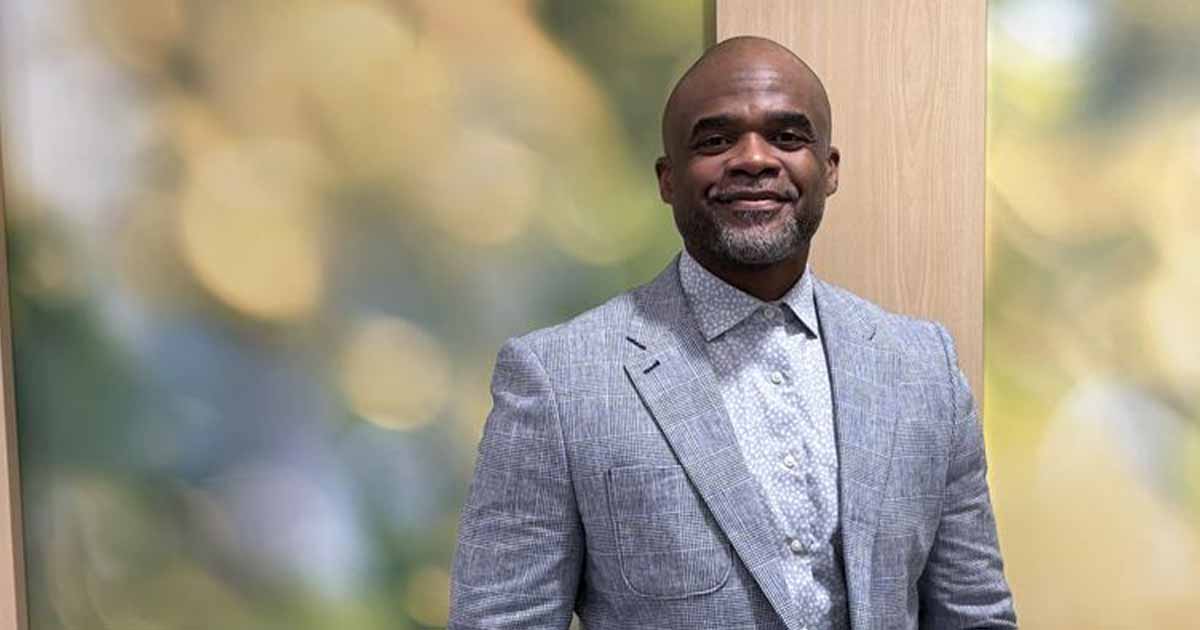
Robert Reedy was bored by his IT job.
After 17 years encompassing various straight IT roles, spanning break-fix to networking, he needed a change. Reedy considered going back to school for nursing, until he found about ONC’s HIT Workforce Development Program, that is.
Reedy, having since graduated from Sinclair Community College’s program in Dayton, OH receives a near-weekly stream of lucrative offers to work as a consultant on EHR implementations.
Government Health IT Editor Tom Sullivan spoke with Reedy about why he wanted to enter the HIT field, the most significant takeaways from ONC’s program, the differences between working in IT for a healthcare organization versus other fields, and ways he think the program could be improved in the future.
Q: Before entering the program you were an IT professional. What specifically was that career?
A: In IT I wore many different hats starting from break-fix to repair and moved into networking with a point of sale company and then moved into another POS company. They do point of sale equipment for grocery store chains and that’s pretty much how I spent 17 years in IT, more on the networking side and small project management and while I was doing that I was a paramedic firefighter part-time and I did that for around 15 years. People sometimes wonder how I ran 15 years with the fire department and also worked in IT the whole time. The schedule became too much to handle with a family and small kids so I had to make the decision a few years back about which to take. I was actually burned out of the IT environment, I hated my job and the career choice. It was so mundane and pretty boring. I needed a change and thought about getting into healthcare and going back to school to bridge my paramedic into nursing when my wife told me about the HIT program at Sinclair College — she was taking radiology there — and I thought it would be a great way to get into medical and I understood IT. It’s been the best move I’ve ever made even though it was kind of scary at 40 years old with mortgages and car payments to uproot my life. Two years later, I couldn’t be happier. I’m so glad I went for it.
Q: The ONC program’s objective is to train IT professionals for healthcare and healthcare pros for IT — as a former IT guy what are the key differences particular to working in healthcare?
A: Right. The healthcare IT side of it, really, other than understanding the workflow of the medical environment and having to approach the network side of it a little bit differently when you have downtime or upgrades or anything that will impact the workflow of clinicians. What seems to be the biggest hurdle is that in a straight IT world you can go in, make changes, do what you need to do and somebody may lose their email or not be able to click on a network or a shared drive. That’s not all that vital. But when you’re in the healthcare industry and have some downtime, clinicians are so dependent on the EMR that it messes up their workflow and you have the added stress that it could impact patient care. So it’s a little more critical to do things on a timeframe that will affect the least amount of people and do it as effectively, efficiently and quickly as possible to limit that downtime. On the healthcare IT side of it, I think, it’s just more demanding to keep things up and running and to make sure your changes are tested and proven before you implement something that is going to completely alter the workflow of patient care providers.
Q: If you are a database administrator or project manager or application developer or network engineer, is the skill set for healthcare actually all that different from other industries?
A: Exactly. As long as you understand the workflow — and I think having a good working knowledge of medical terminology helps — but just the workflow in general along with understanding how big the impact is when you make a change or understanding that you can’t just up and take something down without making sure everybody’s aware of it, making sure that it’s at a point in time where things may be slower. Tuesday at 2 o’clock in the morning is a much better time for something to be deployed than Friday night at 11:30 or 1:30 in the morning when your ED is hopping. In-patient may be slow but you have to worry about the emergency environment. On that same token, if you do it at 10:30 in the morning your ED may be slow but your in-patient’s really buzzing and it’s a juggling act to try and make sure you do things at a slow time — which there’s really not a slow time. It’s fun, it’s exciting, it’s a little — actually it's a lot of pressure — but it’s really rewarding because now you feel like when you build something like the Epic systems we’re building here at Ohio Health, we’re getting ready to start, it’s a real sense of accomplishment seeing the product that you design and build actually being used in a patient care setting and seeing your best practice advisories pop up for certain things. That’s a lot more rewarding that straight IT work is.
Q: That's an interesting point because I was speaking with some folks the week before last who said that Java developers, for instance, are hard to find in healthcare because it’s just not that sexy to a programmer…
A: And my experience to this point has been all end-user support. I watched the builders create things that come to life in a real-world environment and now I’m on the build side and since I’ve seen it from the end-user side it’s very rewarding when I get something, like the best practice advisories we just built, I actually got to see them fired up to work so I know how they function in the real world. I get a great sense of accomplishment. Coming from 17 years of just the strictly IT, health IT gives me a greater sense of accomplishment. Other people who have been in the industry for a while may disagree, or it may be just another job for them but for me because I put a lot on the line just to get here, it’s frankly very rewarding.
Q: We’ve talked about the challenge of understanding the workflows in healthcare, how did the ONC program equip you for that?
A: The biggest thing I took away was the backstory about the buildup to EMRs — why we’re doing that, what the impact will be over the next few years, the meaningful use side of it —because most people that interviewed me were not 100 percent sure what meaningful use was or didn’t understand the impact of it. So I think that in and of itself gave me a huge leg up.
But then the soft skills we learned from Raymond Gooch, an instructor who I still carry on a relationship with to this day, he’s a great person and teacher. The soft skills he taught us are probably the biggest thing I took away from it. The soft skills are kind of the same in the straight IT world but you’re interacting with doctors, nurses, nurse practitioners and all the care providers, so their job’s a little more critical than, say, the manager at a local grocery store. Understanding that you are talking, working and conversing with somebody that at that level is responsible for life and death in the hospital tends to take on a whole new meaning. So learning the ins and outs and sometimes what not to say to a neurosurgeon or a cardiovascular specialist is just as vital as knowing what to say.
Q: Now, in your experience, even anecdotally, are most of the graduates having the same success that you are?
A: I know four people working in the industry at that level. I know of another person that’s become certified on Epic and I know two or three other people that are working in HIT and a couple others were already in a health network when they started the class. I also know people who took classes after me and quite a few of them that became certified for Epic, McKesson or Cerner implementations. I don’t know that it’s as large a group as we’d hoped it would be. It’s weird because it’s such a big undertaking, the whole electronic medical record world, but it’s kind of small when you start talking to people, linking up with them on social media networks, and I have friends I’ve worked with for now about two years who are in California, New Mexico or Texas, Arizona, all over the country and they’ve all gone through the ONC program and are doing a lot more than I am. So in the big picture overall it's working really well. It’s like anything else in that you get out what you put into it and a lot of them seemed to have the misconception that employers were going to beat down their doors and that just didn’t happen. So you really have to do some legwork after the program. But you can go get a masters in anything and then if you stop there and don’t keep the wheels turning people aren't likely to hunt you down just because of the program. So that might be the biggest difference between where some of the people in the class are today.
Q: In at least one story about the program, you’re quoted as saying that you routinely turn down 6 figure jobs — which makes me think that anyone doing that in any field is indicative of there being a lot of jobs out there …
A: Those six-figure jobs are not full-time gigs, they’re consulting roles. But every consulting offer that comes my way is minimum $60 per hour and on up to $120. There’s so much opportunity out there and they’re practically begging people but at the same time you kind of have to get that first go-live under your belt to really see the doors explode. So, I would say I get 10 job offers a week and 90 percent of those are over $55 per hour.
Q: How could the program be improved moving forward?
A: I would say if there was a way for the program to incorporate more internships with local hospitals. It doesn’t even have to be a go-live scenario, just some type of internship where you’re seeing the product and the end-user stage of it. That would probably be extremely helpful because it doesn’t matter which product you’re using, whether it be Epic or Cerner, Allscripts, McKesson. As long as you’ve seen one of them, everybody’s willing to bring you in. I got lucky because my first go live was with Epic, which was the product I wanted to learn so I took for what it was: a 4-week go live. But it opened doors that I couldn’t imagine two years ago.
Related:
AMA says EHRs create an "appalling Catch-22" for docs
Q&A: On health data 'we can't dream big enough'
Commentary: Health policy and implementation challenges to achieving Big Data outcomes