Electronic Health Records (EHR, EMR)
SPONSORED
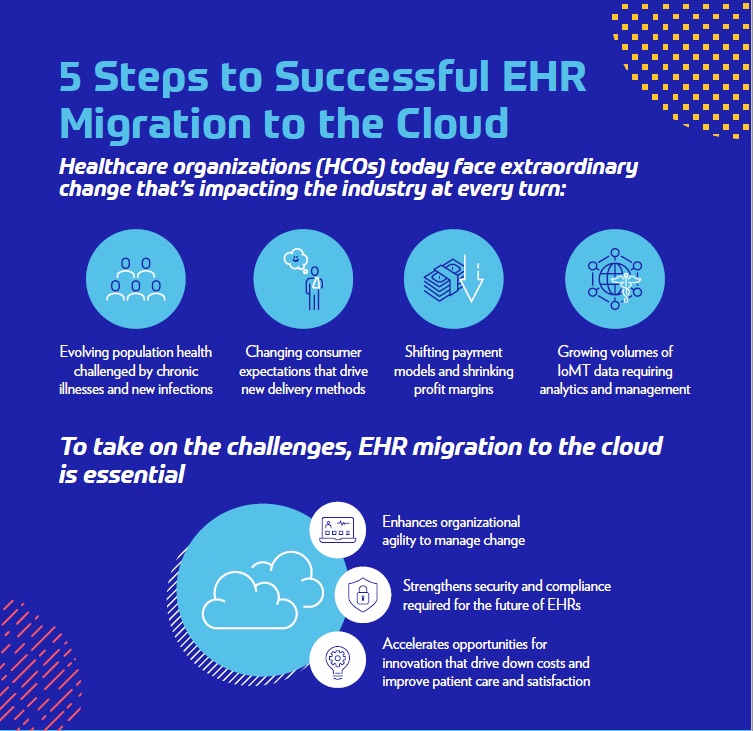
Healthcare organizations are facing extraordinary change that’s impacting the industry at every turn, including changing consumer expectations, shifting payment models and growing volumes of IoMT data requiring analytics and management. Migrating EHR systems to the cloud can enhance an organization’s agility, as well as strengthen security and accelerate opportunities for innovation. Learn how healthcare organizations have realized cost savings and have met organizational goals more readily after moving their EHRs to Azure.
SPONSORED
Healthcare organizations must be able to pivot quickly and respond to today’s ever-changing environment. An increasing number of organizations are moving their electronic medical records (EMRs) to the cloud as part of their digital transformations. Why? The cloud offers a means to update aging infrastructure and also adopt modern EMR technology that can help improve outcomes. Large health systems, including Mount Sinai Health System in New York City, are recognizing the value of moving clinical applications, including EMR, to the cloud.
AHRQ is helping the transition towards evidence-based recommendations to guide clinical decision-making that incorporates patients' needs and preferences.
At Penn Medicine, agile methods have been adopted by a number of information technology teams, including teams that support its enterprise EHR, data analytics, IT operations and systems administration.
EHR deployment in the cloud can help HCOs shift their resources from managing IT infrastructure to improving care coordination, revenue cycle management and patient outcomes.
SPONSORED
Having a proactive, comprehensive disaster resiliency plan that identifies, protects against and detects threats can avoid or minimize the impacts of disasters of all sizes.
Provider burnout has become a $4.6 billion a year problem, resulting in patient and provider churn and a growing physician shortage due to those leaving the profession. Reducing the time that physicians spend documenting patient visits can help decrease fatigue and burnout, as well as allow physicians more time to spend with patients.
Today’s physicians face some unique challenges. Patients are increasingly seeing reduced engagement from physicians who are often rushed and distracted during visits because of the documentation burden, leading to 71% of surveyed patients feeling “frustrated” with their healthcare experience. And with the added frustrations of stressful platform toggling in the shift to telehealth and reimbursements denied due to inaccurate or insufficient documentation, 64% of U.S. physicians say the pandemic has intensified their sense of burnout.
Using their mobile device, physicians unobtrusively record their visits, streaming their speech to the Nuance AI platform, where it gets translated into a clinical node and goes through a quality review process to ensure accuracy before being entered into the EHR. The physician then simply has to review and sign off on the notes, saving time and reducing physician fatigue and burnout.
Scribe programs started with the idea of reducing the data-entry burden on physicians, but high turnover and lack of industry standards and certification for scribes can lead to inconsistent documentation quality and an additional training burden on the physician.