Asia-Pacific hospitals, especially small and medium ones, are financially constrained from adopting emerging technologies like artificial intelligence, based on initial findings from an ongoing study by HIMSS.
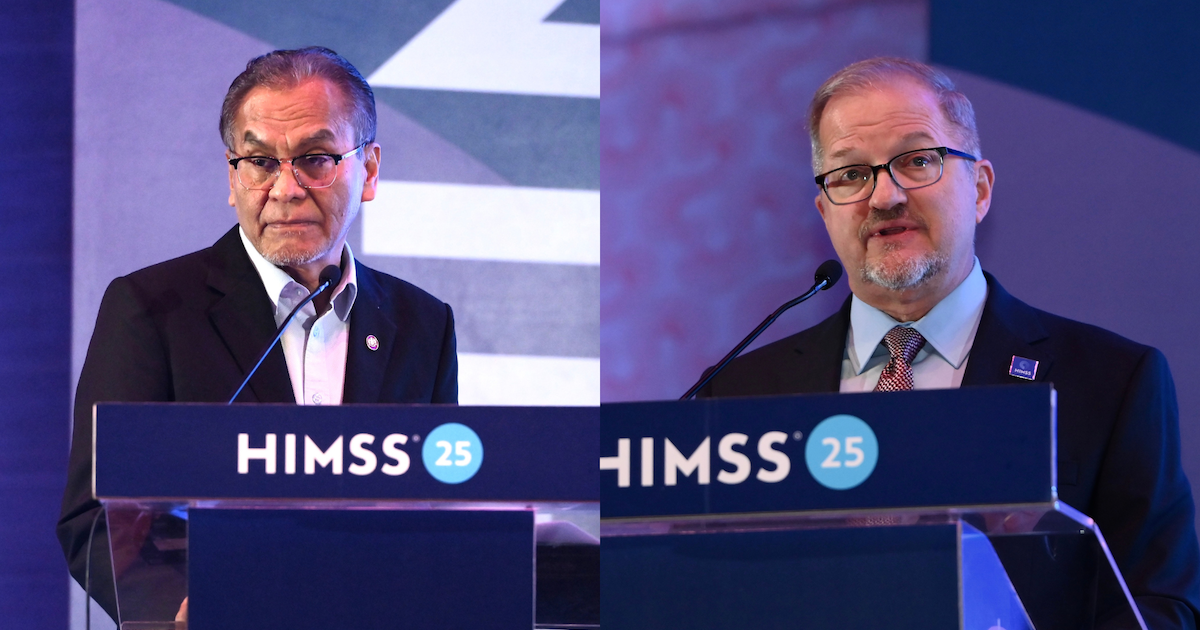
A panel at HIMSS25 APAC discussed these emerging findings from the survey that looked into the state of AI implementations in the APAC healthcare scene.
The panel was joined by Dr Gao Yujia of Singapore's National University Health System (NUHS), Dr Chia Te-Liao of Chi Mei Medical Center in Taiwan, and Dr Seyoung Jung of Seoul National University Bundang Hospital (SNUBH) in South Korea.
Shirley Golen, global head of business development of Amazon's Inclusive eXperiences & Technology program, also participated.
According to Dr Gao, NUHS assistant group CTO, non-tertiary and academic research hospitals, such as district hospitals and primary care clinics, "inherently [have] less funding and budget for AI projects."
"The financial models for the healthcare system at this point in time inherently put restrictions [on] who can or cannot afford AI systems, or what they want to deploy and what they choose to deploy in the hospital itself," he said, explaining why a majority of survey respondents possibly considered financial cost as the biggest barrier to AI adoption in their hospitals.
To encourage greater hospital investment in AI, Amazon's Golen proposed considering "low-hanging fruit" use cases that are easily deployable. These, she said, may involve low-risk or high-impact use cases, such as in administrative state or workflow optimisation, pay-as-you-go cloud solutions, and partnerships with other hospitals.
Dr Jung, associate professor and director of SNUBH's Office of Hospital Information, also suggested looking into plug-and-play AI products, which can be cost-efficient to integrate.
But how can hospitals rationalise the allocation of resources toward AI implementations? Dr Gao said, "Demonstrate the returns, look at not just one or two years, but a three, five, or 10-year roadmap and 10-year returns in order for us to look at the long game and not just a short game."
Meanwhile, Dr Liao, who is the director of Chi Mei Medical Center's Center for Evidence-Based Medicine and Health Policy, added that culture is also an important factor to address. "Trust and the accuracy rate influence the AI adoption in our hospital," he shared.
In Taiwan, three AI centres for healthcare have been established to support hospitals in the safe adoption and implementation of trustworthy AI products. These are the Center for Responsible AI in Healthcare, the Center for External AI Validation in Healthcare, and the Center for Clinical AI Impact Evaluation.
But the biggest barrier to AI adoption, according to Dr Liao, is digitalisation. "In some hospitals [across APAC and Taiwan], they still use papers to write notes and they don't have a hospital information system, [which makes] it difficult to introduce an AI system into their hospitals."
Who covers for healthcare AI risks?
The panel also addressed the uncertainty among healthcare professionals over errors and omissions insurance related to AI use.
"Although AI has advanced in recent years, I still think AI is not mature [enough] to be included in commercial insurance because [we] don't know to whom [we] should pay – the doctor or the patient," Dr Liao said.
A comprehensive evaluation mechanism or framework, he said, is needed to assess insurance coverage for AI-related risks in healthcare. He noted how one of the Taiwanese government's AI centres – the Center for Clinical AI Impact Evaluation – is looking to include the evaluation of insurance covers for AI risks.
While near misses or adverse events involving the use of AI are not impossible, the added scrutiny on AI may not be warranted, as these could also happen without the use of the technology, stressed Dr Gao.
"[AI] is not that much different from what we've been deploying and implementing so far."
Both Drs Jung and Gao referred to the example in the automotive industry where car owners are given discounts in insurance premiums for their installation of AI-driven safety features.
"A lot of newer cars actually have AI-driven systems inside – for example, anti-collision and lane departure warnings, and they are [priced] at a much lower insurance premium than older cars with no AI," explained Dr Gao.
"This is kind of the reverse of what most people are saying in the medical field, where the inclusion of AI potentially increases the insurance premiums patients pay."
Dr Gao suggested rethinking how the use of AI and its impact on healthcare delivery is interpreted. "We need to look at how the utilisation of AI can potentially affect insurance coverage."
"The final care decisions are done by physicians [themselves]... But I hope someday, given AI's benefits, insurance companies would give us some reimbursement from our use of AI software, in clinical settings," Dr Jung also said.